Meeting the moment
UTHealth Houston stroke experts harness ingenuity and philanthropy to save lives
In stroke care, the difference between life and death can be the blink of an eye. Without access to prompt diagnosis and treatment, a stroke victim can lose up to two million brain cells per minute. The second-leading cause of death worldwide and one of the leading causes of disability, strokes continue to grow more common as our population ages and more people develop chronic conditions.
Across UTHealth Houston, clinicians and researchers are working together to build a deeper understanding of how to prevent, diagnose, and treat stroke, but time is of the essence. The likelihood of suffering a stroke continues to increase, and our communities need better access to elite stroke care. Fueled by philanthropy, UTHealth Houston stroke experts are meeting this moment by harnessing new technologies and data to save and restore lives.
As soon as Rich Majeres started losing vision—a hallmark of the migraines he has endured since childhood—he reached for the medication in his office desk. One quick dose could always clear things up and prevent a blitz of head-splitting pain that could blot out his day. But this time, the drum in his brain only pounded stronger as his surroundings blurred.
“I think I need to go home and sleep this one off,” he told his wife, Kasi, who worked part-time at his accounting firm. It was an unusual comment; Rich often amassed 80 hours per week building business at his new firm, and he rarely missed time, with or without a migraine.
While Kasi drove Rich home, their daughter called from college. Not wanting to miss a chance to talk, Rich held a conversation between the pulses of pain until they arrived home. At the end of the call, he repeatedly tried to hang up the phone in the car door.
“I just remember staring at the phone in my hand and thinking something isn’t right,” he says. “I tried to get out of the car and couldn’t lift my legs. From there, things get cloudy.”
Kasi recognized Rich was suffering a stroke and called 911. Responders dispatched the UTHealth Houston Mobile Stroke Unit, which arrived in five minutes. Thanks to the unit’s onboard CT scanner, the UTHealth Houston care team quickly learned Rich was having an ischemic stroke—one caused by a clot blocking blood flow in the brain— and administered the clot-dissolving drug, tissue plasminogen activator (tPA).
Once Rich arrived at the hospital, Sunil A. Sheth, MD, vascular and interventional neurologist at UTHealth Neurosciences and McGovern Medical School at UTHealth Houston, discovered the clot still blocked precious oxygen from reaching Rich’s brain. With time running out, he needed surgery to remove the clot in order to survive.
Rich learned he had a stroke when nurses removed his breathing tubes after the 4.5-hour surgery. He remembers thinking it farfetched that this could happen to him: a healthy, active 53-year-old who lacked most of the associated risk factors like obesity, smoking, and diabetes.
“I grew up working long days on my family’s dairy farm, and I’m accustomed to hard work and leading an active lifestyle,” he says. “While my job was demanding and frequently required late nights, I managed the stress by exercising and playing in a weekly softball league. Having a stroke was like being struck by lightning.”
A stroke can strike anyone at any time, and response time often means the difference between life and death. The quick reactions from Kasi, the UTHealth Houston Mobile Stroke Unit, and Sheth led to a nearly full recovery for Rich, aside from some weakness and pain in his left arm.
“Everything fell into place the day of my stroke, and I received the best possible care as fast as possible,” says Rich. “I wouldn’t be here without the fast response from the Mobile Stroke Unit and the surgical expertise of Dr. Sheth.”
Although rapid diagnosis and intervention saved Rich’s life, many patients live in areas that lack immediate access to elite stroke response and care. In fact, 84 out of 254 counties in Texas do not have a hospital.
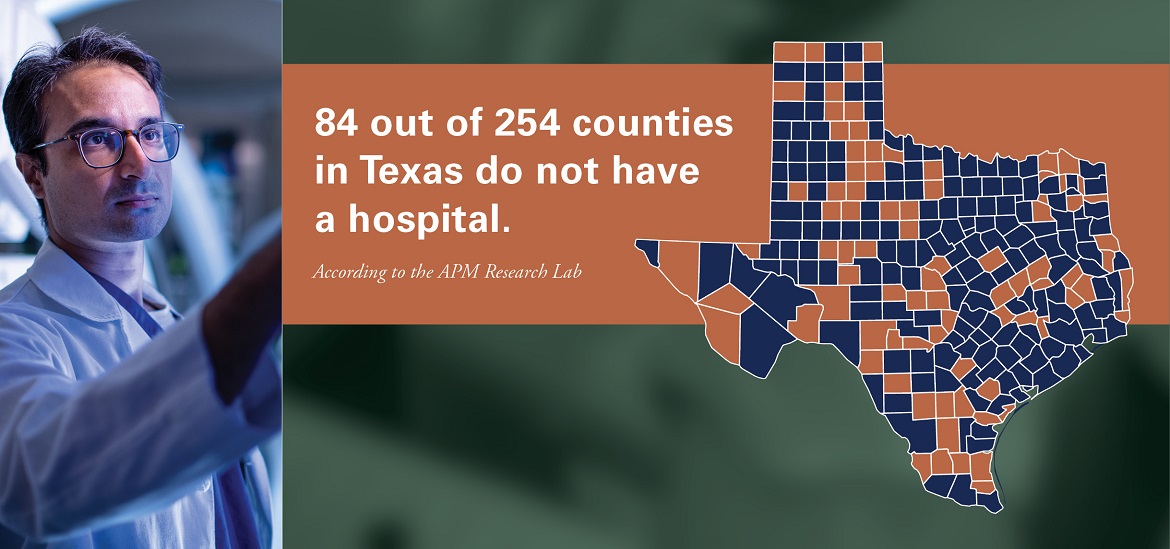
Texas counties without hospitals
The infographic depicts a map of Texas that highlights the 84 counties that do not have a hospital.
Embedded text: 84 out of 254 counties in Texas do not have a hospital.
Across UTHealth Houston, researchers are pursuing innovative studies to make a meaningful difference in the lives of stroke patients and survivors— whether they live in cities or rural communities. Sheth works with Luca Giancardo, PhD, and researchers at UTHealth Houston School of Biomedical Informatics to speed up the diagnosis and treatment of stroke through artificial intelligence.
They developed an algorithm that uses a dye injected into the body and CT imaging—readily available at smaller hospitals—to rapidly identify a common type of ischemic stroke similar to the one Rich suffered. The team is also investigating an alternative way to diagnose stroke using common retinal cameras placed in ambulances to photograph the inside of the eye.
“Behind all our work, our goal is to make elite stroke response and care more accessible for everyone,” says Sheth. “We want people to be able to receive the best quality screening and treatment, no matter who they are or where they are.”
Experts like Sheth and Giancardo are part of the UTHealth Houston Institute for Stroke and Cerebrovascular Disease. UTHealth Houston, with Memorial Hermann-Texas Medical Center, was one of the world’s first stroke centers and leads the Gulf Regional Area Stroke Program, one of the nation’s largest National Institutes of Health-funded stroke networks. Working in concert with the Stroke Institute, clinicians and researchers from UTHealth Houston, Memorial Hermann Health System, and the Texas Medical Center work together to better understand and treat stroke and other cerebrovascular diseases.
In stroke research—just like in stroke treatment—time proves crucial. Philanthropy can ignite collaborations like those at the Institute for Stroke and Cerebrovascular Disease and spark innovative research programs that lead the way for comprehensive stroke care across the full spectrum—from prevention to rapid response and recovery.
For instance, philanthropy is helping researchers freeze moments during and after a stroke to study the tiniest details—like capturing bolts of lightning in jars.
In December 2017, a substantial contribution from the Huffington Foundation enabled Louise D. McCullough, MD, PhD, to launch the BioRepository of Neurological Disorders Registry and Tissue Repository. The BioRepository stores genetic information, blood samples, urine, cerebrospinal fluid, and brain biopsy tissue from patients who suffer stroke or other neurological conditions, enabling researchers across the university to launch innovative projects to discover molecular pathways of diseases and develop new treatments.
The BioRepository stands out not only because of the samples it holds, but also because of who runs it: medical students and gap-year students—those between undergraduate studies and graduate or medical school.
“The students who run the BioRepository represent the future of neurology,” says McCullough. “Exposing young scientists to clinical and discovery research provides unparalleled experience and helps shape their future careers.”
For Yashee Munshi, a second-year student at McGovern Medical School, working at the BioRepository during a gap year was a way to learn more about a condition that impacted her family. It also solidified her decision to pursue a career in medicine.
“After my father suffered a stroke, I wanted to learn more about it and make a difference for other families,” she says. “The BioRepository showed me how research can improve care for patients. We see areas at the patient bedside that need improvement, and we turn those things into research projects.”
In addition to serving as a launch pad for neurological research, the BioRepository also contributes to UTHealth Houston’s COVID-19 response efforts. At the onset of the pandemic, McCullough rapidly converted the BioRepository to collect samples from patients hospitalized for COVID-19 after a positive test. It now holds samples from more than 700 patients that researchers from around the world can study.
“The generosity of donors allows us to scatter seeds and see what grows,” says McCullough. “Philanthropy is the key to innovation, whether allowing us to jumpstart high-risk, high-reward projects or helping us to recruit the brightest students and trainees.”